Osteoporosis is a global health epidemic, according to the World Health Organisation (WHO).1 With over 200 million people affected by clinical bone loss, most of which are women, osteoporosis is now only second to cardiovascular disease as a global healthcare problem, with fragility fractures sending the risk of premature death rising by 50%.2
Being nicknamed “the silent disease” due to its slow and typically asymptomatic progressive nature, most people are unaware they are at risk of osteoporosis until either a fracture occurs or it is unexpectedly detected on medical imaging or a DEXA scan. As such, many people are now placing their bone health at the top of their priority list and taking self-directed steps to understand their risk factors and proactively care for their bone health.
Here is a look into what osteoporosis is, its risk factors, and what you can do to reverse the damage and care for your bone health.
What Is Osteoporosis?
Literally translating to “bones with holes”, osteoporosis is a condition that is diagnosed when your bone mineral density, meaning how much calcium and other types of minerals are present in an area of your bone, is significantly reduced – approximately 2.5 standard deviations or more below the average value, according to WHO criteria.3 Simply put, when your normally dense and mineral-filled bones lose enough of this mineral ‘filling’ that it leaves them significantly weaker and more vulnerable to fractures, osteoporosis is present.
There is also a condition called osteopenia, often nicknamed ‘pre-osteoporosis’, which means that your bone mineral density has decreased below normal values, but is not yet low enough for you to be formally diagnosed with osteoporosis.4 Osteopenia is a big warning sign that osteoporosis is not far behind if your current daily activities and attention to bone health do not improve.
Getting into the specifics, there are two types of osteoporosis. Primary osteoporosis is seen in post-menopausal women, and older women and men. Secondary osteoporosis occurs secondary to diseases, treatments or an idiopathic (unknown) process at any age. Examples include endocrine and systemic diseases.5
To answer the question of why you lose bone mineral density, your bone cells are constantly being broken down and renewed by the body. When bone is being broken down at the same rate at which it is renewed, your bones maintain their current density. When renewal happens faster, as it does naturally in our younger years, more bone is built. And when more bone is lost than replaced, you lose bone mineral density.
When your bones are thin and fragile, your risk for fractures significantly increases, both in traumatic fractures, meaning the risk of sustaining a fracture following an injury or event like a fall, and in fractures sustained from regular everyday activities. Once you have one fracture, your risk for another skyrockets, while being linked to a lower quality of life,6 health status, impaired physical function and increased pain.7 This is why doing everything you can to care for your bone health and prevent osteoporosis, as early as possible, must be a critical part of a person’s health management plan.
Osteoporosis Risk Factors
The risk factors for osteoporosis fall into two categories: those that are modificable, and those that are non-modifiable.
Modifiable risk factors for osteoporosis
Modifiable risk factors are the ones that you have at least some control in changing to be able to better improve your bone health. These are the ones that must be addressed when you are looking to prevent osteoporosis, improve your bone health, and stop a diagnosis of osteopenia from progressing to osteoporosis. They include:8,9
- Physical inactivity
- Calcium deficiency from your diet
- Long-term glucocorticoid (steroid) use
- Smoking
- Being underweight with a low BMI
- Hypogonadism
- Inadequate vitamin D intake
- High alcohol intake
- Poor nutrition
- Stress
Non-modifiable risk factors for osteoporosis
Non-modifiable risk factors are the ones you can’t control and include:10
- Your gender (particularly being female)
- Entering menopause or having a hysterectomy
- Age
- Race
- Genetic characteristics
- Taking certain medications that are essential in treating other medical conditions including thyroid hormone supplements, certain diabetes medications, anti-coagulants, certain chemotherapy agents, proton pump inhibitors, certain immunosuppressants and more
- The presence of other diseases including rheumatoid arthritis, cancer, kidney disease and more
As mentioned, previous fractures are also notable risk factors. The earlier the age at fracture and the greater the number of previous fractures, the greater the subsequent risk. The risk of vertebral fractures is at least two-fold in those with previous vertebral fractures. A wrist fracture doubles the risk of hip fracture and triples the risk of vertebral fracture.11
Is Osteoporosis Reversible?
This depends on how technical you want to be, and different medical organisations hold different interpretations of this term. If ‘reversible’ implies restoring the health of a 70-year-old bone to its 30-year-old density, strength and function, then no – osteoporosis is not reversible. However, there are many things you can do to slow bone loss, improve it, and even help strengthen and rebuild bones. So if your definition of reversing osteoporosis means to improve your bone health and stop the process by which you continue to lose bone, then yes, you can achieve stronger, healthier bones, improve your quality of life, and reduce your fracture risk.
Evidence-based Ways To Prevent Osteoporosis Or Improve Bone Health
Preventing osteoporosis and improving your bone health follow the same principles: adjusting your modifiable risk factors while proactively taking further actions that support your bone health. Managing your modifiable risk factors can look like:
1. Exercising Regularly
While being told to exercise regularly is a common piece of advice that is often not heeded, weight-bearing exercise is proven to be a treatment and prevention method for both postmenopausal and age-associated osteoporosis.12 Incorporating various forms of physical activity into our daily lives is shown to improve muscle function and offset age-related muscle morphology changes.13 To best benefit from the results, the National Osteoporosis Foundation recommends skeletal loading with high and low-impact weight-bearing exercises for at least 30 minutes per day, 5–7 days a week.14
2. Improving your diet
It is widely known that calcium and vitamin D intake are necessary for good bone health, however, research from the Framingham Osteoporosis Study on over 5,000 adult men and women have shown that various other foods and nutrients play an important role in bone health too,15 including vitamin C, carotenoids, folate and B12, vitamin K, potassium, magnesium, fish (three or more servings per week), omega-3 fatty acids, dairy products (whose nutritional benefits go above calcium and vitamin D to include magnesium, zinc, riboflavin and protein), protein, and more. You can read more about this here.
3. Avoid smoking & limiting alcohol intake
Smoking & alcohol can inhibit new bone development, impair hormone regulation and speed up bone deterioration. In women, smoking can decrease estrogen level and this is directly linked to bone health. Refraining from both has been shown to improve markers of bone density.
4. Stopping unprescribed steroid use
5. Maintaining a healthy BMI
6. Managing stress levels
Taking further actions to support your bone health
Beyond the modifiable risk factors, you can also take proactive steps to support your bone health. There are two primary ways to achieve this:
Medications for osteoporosis
There are a range of different medications available for osteoporosis based on your unique circumstances and other medical conditions, and they have varying mechanisms of action. Common brand names include Fosamax, Actonel, Boniva, and Reclast. You may be prescribed an antiresorptive drug that slows the rate that your body breaks down bone, or an anabolic drug that increases bone formation.
The use of medications for osteoporosis shows promising results in helping reduce the prevalence of fractures, though they pose some notable barriers. Aside from the risk of adverse effects16,17 meaning they require very carefully prescription, research has found osteoporosis medication to be associated with poor patient adherence18,19 leading to poor outcomes. A study examining the attitudes and treatment patterns of Australian GP’s in treating osteoporosis found that in over 80% of cases where patients ceased their medication, prescriptions were not being followed up or continued, placing these people at risk of further fractures and suggesting that osteoporosis was undertreated and underdiagnosed.20
Low intensity vibration for osteoporosis
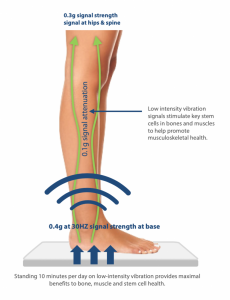 Low intensity vibration (LiV) has been found to promote the construction of healthy bone and muscle, and inhibit the formation of fat, improving bone outcomes in patients.21 Whole body vibration (WBV) between 20-90Hz in animals has been found to promote the generation of bone and muscle, preventing and reversing osteoporosis.22 Moreover, 30Hz vibrations have been shown to build bone and muscle in the hip and spine of young women with osteoporosis23, promote volumetric bone density in the proximal tibia of children with conditions such as cerebral palsy24, enhance bone quality in adolescents with idiopathic scoliosis25, and help protect balance control in those subject to chronic best rest.26
Low intensity vibration (LiV) has been found to promote the construction of healthy bone and muscle, and inhibit the formation of fat, improving bone outcomes in patients.21 Whole body vibration (WBV) between 20-90Hz in animals has been found to promote the generation of bone and muscle, preventing and reversing osteoporosis.22 Moreover, 30Hz vibrations have been shown to build bone and muscle in the hip and spine of young women with osteoporosis23, promote volumetric bone density in the proximal tibia of children with conditions such as cerebral palsy24, enhance bone quality in adolescents with idiopathic scoliosis25, and help protect balance control in those subject to chronic best rest.26
The best LiV tool currently available on the market is the Marodyne LiV. Marodyne is a modern device that has been recognised by the Royal Osteoporosis Society as a safe and effective tool for the prevention of osteoporosis and the improvement of bone health. Its mechanism of action is grounded in the principles of exercise, where the musculoskeletal system responds to ground reaction forces, loading a person’s bone tissue with high and low frequency mechanical signals. The ability of these mechanical signals to increase musculoskeletal mass and quality is multifactorial, simultaneously repressing the systems involved in the formation of adipose tissue (fat), while also promoting the construction of bone.27 By increasing both muscle and bone mass and strength, exercise is able to reduce the incidence of bone fractures.
Marodyne does not require a prescription, is safe to use at home, and is suitable for both prevention in healthy individuals and for treatment for those with weaker bones. Doctor Clinton Rubin Ph.D. is a distinguished State University of New York professor and a global authority on vibration therapy, whole body vibration platforms and their impact. He recommends a minimum of 10 minutes per day, citing that the most important component for success is not duration, but consistency. Using the Marodyne LiV every single day is a more important factor than the time for which it is used. A growing evidence suggests that the incorporation of multiple cycles of mechanical signals within a given day, separated by periods of rest, can increase the beneficial bone-building effects.28
How To Start Improving Bone Health Today
You can start improving your health, managing your osteoporosis, and reducing the risks of it developing by starting with your modifiable risk factors today. Together, we recommend the use of Marodyne Liv due to its position as a simple, easy and effective solution for osteoporosis. It can be utilised by all age ranges, all physical abilities, without the need for repeat prescriptions or GP visits, and without strenuous or unmanageable exercise.
Marodyne LiV is available exclusively from Rehacare. To purchase the device, or for any questions please contact Marodyne LiV Australia on 1300 653 522 or at sales@rehacare.com.au.
[1] https://www.nbihealth.com/osteoporosis-global-health-crisis/
[2] https://asbmr.onlinelibrary.wiley.com/doi/full/10.1002/jbmr.3118
[3] https://josr-online.biomedcentral.com/articles/10.1186/s13018-021-02772-0
[4] https://www.ncbi.nlm.nih.gov/books/NBK499878/
[5] https://josr-online.biomedcentral.com/articles/10.1186/s13018-021-02772-0
[6] https://www.tandfonline.com/doi/full/10.1080/21556660.2019.1677674
[7] https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-019-1268-y
[8] https://www.racgp.org.au/afp/2012/march/osteoporosis-prevention-and-detection
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6225907/
[10] https://www.osteoporosis.foundation/patients/about-osteoporosis/risk-factors
[11] https://www.sciencedirect.com/science/article/abs/pii/S0378512298000905
[12] https://pubmed.ncbi.nlm.nih.gov/30814687/
[13] Rogers, M. A. & Evans, W. J. Changes in skeletal muscle with aging: effects of exercise training. Exerc. Sport Sci. Rev. 21, 65–102 (1993).
[14] https://cdn.nof.org/wp-content/uploads/2016/02/Exercise-for-Your-Bone-Health.pdf
[15] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4928581/
[16] https://pubmed.ncbi.nlm.nih.gov/30814687/
[17] Rossouw, J. E. et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA 288, 321–333 (2002).
[18] Siris, E. S. et al. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin. Proc. 81, 1013–1022 (2006).
[19] Cramer, J. A., Gold, D. T., Silverman, S. L. & Lewiecki, E. M. A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos. Int. 18, 1023–1031 (2007).
[20] https://bmcfampract.biomedcentral.com/articles/10.1186/s12875-020-01103-2
[21] https://pubmed.ncbi.nlm.nih.gov/30814687/
[22] https://pubmed.ncbi.nlm.nih.gov/15597385/
[23] https://pubmed.ncbi.nlm.nih.gov/16939405/
[24] https://pubmed.ncbi.nlm.nih.gov/15040823/
[25] https://pubmed.ncbi.nlm.nih.gov/23011683/
[26] https://pubmed.ncbi.nlm.nih.gov/21273076/
[27] Wallace, B. A. & Cumming, R. G. Systematic review of randomized trials of the effect of exercise on bone mass in pre- and postmenopausal women. Calcif. Tissue Int. 67, 10–18 (2000).
[28] https://pubmed.ncbi.nlm.nih.gov/30814687/



